Comprehensive meta-analysis from IFFO partner GOED helps clarify the science on omega-3s and human health
By Chris Gearheart
Director – Member Communications and Engagement at GOED, The Global Organization for EPA and DHA Omega-3s
A new study published in September in Mayo Clinic Proceedings online, “Effect of Omega-3 Dosage on Cardiovascular Outcomes: An Updated Meta-Analysis and Meta-Regression of Interventional Trials,” shows a connection between an increase in omega-3 intake and a variety of cardiovascular risk reductions.
The meta-analysis, commissioned by IFFO partner organization GOED, the Global Organization for EPA and DHA Omega-3s, is the most comprehensive study combining all the human clinical trials to date on the topic (40 clinical trials with more than 135,000 subjects). It found that EPA and DHA supplementation is associated with statistically significant reductions in several cardiovascular outcomes:
- 35% reduced risk of fatal myocardial infarction (MI)
- 13% reduced risk of MI
- 10% reduced risk of coronary heart disease (CHD) events
- 9% reduced risk of CHD mortality
Research Then and Now
As background, EPA and DHA omega-3s have been researched for their human health benefits for decades. In the 1970s, scientists Jorn Dyerberg and HO Bang found that native Greenlanders who ate traditional diets high in marine fats tended to have more EPA and DHA in their blood and experience less cardiovascular disease. Then from 1980 to 2011, scientists published more than 21,000 papers on EPA and DHA — 2,554 of which were clinical trials — mostly showing a positive correlation between EPA+DHA consumption and heart health.
In 2012, a large-scale clinical trial called ORIGIN studying heart health outcomes in 12,536 diabetics and prediabetics interrupted the positive trend, finding no significant heart health benefit of EPA and DHA consumption. Furthermore, one of the authors, Dr. Evangelos Rizos, published one of the first meta-analyses on the topic during the same year, arguing that the previous body of research had not proved a cardioprotective effect for omega-3s.
After 2012, clinical trials and other meta-analyses continued to demonstrate contradictory findings and mainstream consumer media reporting on the studies began to publish headlines questioning omega-3’s effectiveness. For several years, few randomized controlled trials (RCTs) on omega-3s and cardiovascular outcomes were published.
Omega-3 research took a huge leap forward in 2018 when three large scale clinical trials on omega-3s were published. The three studies — ASCEND, VITAL and REDUCE-IT — more than doubled the number of subjects who had been studied for the impact of omega-3s on cardiovascular outcomes. This introduced the possibility of analyzing the impact of omega-3 dosage on cardiovascular outcomes and led to the current meta-analysis.
The Dosage Connection
The Mayo Clinic Proceedings paper, which was co-authored by Aldo Bernasconi, PhD, Vice President of Data Science at GOED, cardiologist Carl “Chip” Lavie of the John Ochsner Heart and Vascular Institute and Ochsner Clinical School and biostatistician Michelle Wiest of the University of Idaho, demonstrated that omega-3 dosage could be correlated with improved cardiovascular outcomes.
Incorporating data from the three 2018 studies along with the prior body of evidence, Dr. Bernasconi et al found that an additional 1 g/day* of EPA+DHA resulted in additional statistically significant risk reductions:
- 5.8% reduction in the risk of cardiovascular disease (CVD) events
- 9.0% reduction in the risk of MI
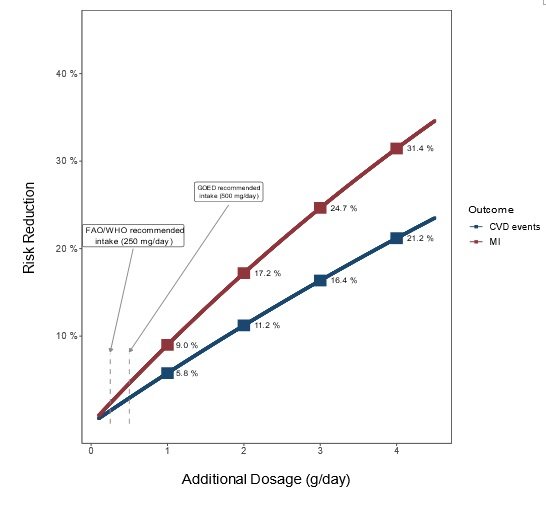
(*The study looked at dosages up to 5.5 grams per day).
According to Dr. Bernasconi, “Each new study contributes a little bit to our understanding of any scientific question. I think this article in particular is the most comprehensive exploration to date of what factors affect the effect of omega-3 supplementation. It found that, unsurprisingly, dosage is the most important factor. Simply put, studies with higher dosages are more likely to find a positive effect. I think that this may help design future studies to have sufficient dosage in order to see a measurable effect.”
The study also has implications for public health. As coauthor Dr. Lavie pointed out, “Considering the relatively low costs and side effect profiles of omega-3 supplementation and the low drug-drug interactions with other standard therapies used in cardiovascular prevention, consumers and physicians should consider the potential benefits of omega-3 (EPA+DHA) supplementation, especially using dosages of 1000-2000 mg/day, which are rarely obtained in most Westernized diets, even those including some routine fish consumption.”
IFFO members who are interested in sharing this information with customers can access a simplified infographic detailing the study here.








